My first workshop at the 2017 Diabetes UK Professionals’ Conference entitled Non-Hungry Eating rang loud bells as I’ve had significant ‘food issues’ myself over the years. I wanted to hear what advice was being offered to clinicians, plus I’m really interested in the type 2 National Prevention Programme as I have a friend who struggled with overeating for years before reversing her type 2 following bariatric surgery.
Led by clinical psychologist Dr Jen Nash of Positive Diabetes (who also has type 1 and had issues with her own eating) and Rosie Walker, a diabetes specialist nurse from Successful Diabetes, the workshop explored how to broach the subjects of overweight and overeating when people are reluctant or unable to acknowledge it’s a problem.
They looked at ways to remove judgement from conversations – thankfully a recurrent theme of the Conference 👍. Jen and Rosie gave examples of sensitive language to encourage ownership of overeating, explored the shame and guilt overweight often brings and looked at triggers for non-hungry eating or bingeing. The links with pre-diabetes and type 2 are obvious, but other presenters also described the increasing prevalence of obesity amongst type 1s, with its consequent risk of blood pressure and cardiovascular problems. According to a slide shown at a later presentation, the UK is 2nd in the European Obesity League (OECD Health at a Glance 2014).  We discussed what Jen called ‘Conversation Stoppers’, how many overweight people claim to eat little, to come from a family of ‘large’ people or to lose weight but regain it easily despite eating little. It’s a bit like alcoholics: only when the problem’s acknowledged can change and recovery begin.
We discussed what Jen called ‘Conversation Stoppers’, how many overweight people claim to eat little, to come from a family of ‘large’ people or to lose weight but regain it easily despite eating little. It’s a bit like alcoholics: only when the problem’s acknowledged can change and recovery begin.
Jen and Rosie described ‘normalising’ overeating to help their patients open up and explore why they do it. And when people are not ready to discuss it, that’s fine, Jen leaves it open so they know she’s willing as and when they want to tackle it – all very reassuring I thought.
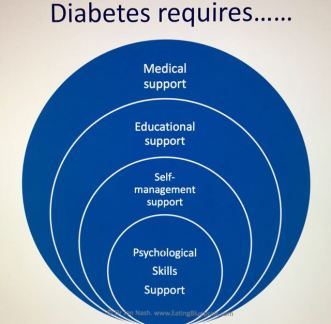
I was grateful that they emphasised how non specialists – practice nurses, GPs and hospital clinicians – should act as signposts and acquaint themselves with referral pathways to psychological support. Clinicians often see weight as the problem when it’s really a symptom of stress that once treated, leaves the way open to address the eating and weight comcerns. Being overweight is a very complex problem and is NOT simply a matter of weak willpower. But the sad fact is that access to specialist support is at best, patchy. Many of us with diabetes need psychological skills along with the diabetes education we get to manage this elephant in the room: food.
 As a clinical psychologist at the Joslin Diabetes Center in the USA said “Teaching a person how to be a ‘good diabetic’ is akin to teaching them how to have an eating disorder”. Too true. Thank goodness it’s more widely acknowledged now – when I sought help with crazy eating behaviour as a teen with type 1, I was given another carb counting list and sent packing…
As a clinical psychologist at the Joslin Diabetes Center in the USA said “Teaching a person how to be a ‘good diabetic’ is akin to teaching them how to have an eating disorder”. Too true. Thank goodness it’s more widely acknowledged now – when I sought help with crazy eating behaviour as a teen with type 1, I was given another carb counting list and sent packing…
It’s reckoned there are 30+ reasons we eat and most are unrelated to physical hunger. They involve what Jen called heart hunger (emotional eating) or eyeball hunger (that looks SO good!). Almost all of the 50+ clinicians at the workshop said they regularly ate when they weren’t physically hungry. It’s pretty normal – we all do it. 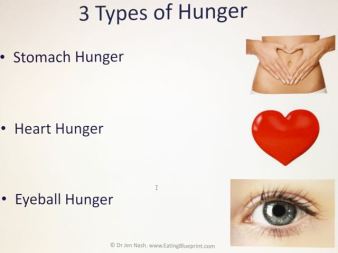 Food makes us feel safe, it can act like a sedative, calming us down when stressed. We sometimes eat to solve problems, but create a bigger one in doing so. I can vouch for the fact that robust psychological skills are needed to overcome overeating!
Food makes us feel safe, it can act like a sedative, calming us down when stressed. We sometimes eat to solve problems, but create a bigger one in doing so. I can vouch for the fact that robust psychological skills are needed to overcome overeating! If eating inappropriately large amounts, whether to manage feelings or not (some do eat for other reasons!), it can make diabetes management very challenging. And if we’re overweight, we’re more resistant to insulin whatever type of diabetes we do or don’t have. Another presentation by Prof Roy Taylor made a strong case for type 2 prevention via strict calorie reduction on a liquid diet, though he did add that a great deal of ongoing support was needed for people to stick to the regime used in his research. It was mentioned that growing numbers of overweight type 1s are now taking Metformin alongside insulin to improve insulin absorbency.
If eating inappropriately large amounts, whether to manage feelings or not (some do eat for other reasons!), it can make diabetes management very challenging. And if we’re overweight, we’re more resistant to insulin whatever type of diabetes we do or don’t have. Another presentation by Prof Roy Taylor made a strong case for type 2 prevention via strict calorie reduction on a liquid diet, though he did add that a great deal of ongoing support was needed for people to stick to the regime used in his research. It was mentioned that growing numbers of overweight type 1s are now taking Metformin alongside insulin to improve insulin absorbency.
Many other presenters spoke about food in relation to weight. A stand out message for me came from Dr Nita Forouhi who, after alluding to every eating style in the dieter’s library, said the only diet that works for weight loss is the one that works for you. She added that all calories are not equal – for long term health benefits it’s vital to consider nutritional variety and quality. So that’s a ‘no’ to the beer and broccoli regime.
And finally, I must mention a talk given by Richard Welbourn, a bariatric surgeon who presented a very compelling case for weight loss surgery. I love his slide Surgeons are Heroes.  He claimed it’s the only treatment that ticks all the boxes in terms of weight loss, type 2 prevention, management and cure, behaviour modification and importantly, improved quality of life for nearly all who undergo procedures. Most of his patients had tried to lose weight for years with various interventions, but hadn’t managed it. He concluded there is no ‘recommended’ procedure – all have risks and benefits that need careful consideration on a one by one basis.
He claimed it’s the only treatment that ticks all the boxes in terms of weight loss, type 2 prevention, management and cure, behaviour modification and importantly, improved quality of life for nearly all who undergo procedures. Most of his patients had tried to lose weight for years with various interventions, but hadn’t managed it. He concluded there is no ‘recommended’ procedure – all have risks and benefits that need careful consideration on a one by one basis.  As Richard’s slide shows, NICE guidelines are in place for those with type 2 but sadly, though there are thousands waiting who could benefit, the barriers to accessing help – lack of belief in the financial and clinical benefits and lack of finance – remain. He sounded like a fighter to me, so watch this space…
As Richard’s slide shows, NICE guidelines are in place for those with type 2 but sadly, though there are thousands waiting who could benefit, the barriers to accessing help – lack of belief in the financial and clinical benefits and lack of finance – remain. He sounded like a fighter to me, so watch this space…
Slides (with exception of last two): Dr Jen Nash http://www.EatingBlueprint.com
Other helpful resources: Food Psychology – Dr Jen Nash
Dr Jen Nash’s Diabetes UK page on non hungry eating
Prof Roy Taylor’s Diabetes UK page on diet and type 2 diabetes
Prof Roy Taylor on reversing type 2 diabetes
Beating EATing Disorders B-EAT
Diabetics With Eating Disorders (DWED)
.

Thank you Lis – another wonderfully wise exposition of the range of views at the conference. It’s sad to learn that obesity in people with type one is rising in line with the population generally, although I got very cross at a Tim Noakes video the other day which was saying that people with type one end up getting type two and vice versa, and at the researcher at the conference who insisted that children with type one shouldn’t be managing activity with carbohydrate (only insulin adjustment). Little advice out there for people like my little T1D who needs to put on a bit of weight so his cannulas have somewhere to go… (recognise he’s the minority though). Great advice in this blog for type zeros (potential future type twos) who need to rethink their disordered eating habits. Very useful.
LikeLike